A medical practice management software (MPMS) is a set of tools that help hospitals, doctors, medical practitioners, healthcare facilities, and healthcare workers manage various aspects of their practice and organization. It includes Electronic Health Records (EHRs), patient scheduling, billings and payments, insurance payer claims, telehealth functions and implementation, practice reporting, e-prescriptions, and many other areas.
Medical Practice Management Systems (MPMS) have been designed to integrate and facilitate the digital transformation of most aspects of a physical practice into a connected digital workspace. All systems are HIPAA-compliant and operate at high-security levels, with high-grade encryption, fault-tolerant servers, and redundant cloud backup.
On the patient side, medical practice management platforms handle the patient portal, patient data and documentation management, pre-registration and scheduling, and all communication. Patient Electronic Health Records (EHR) or electronic medical records (EMRs) are digital versions of a patient’s paper charts and documents. On the business side, the standard features of MPMS are payment processing, billing, and claims processing. Usually, the financial parts of your business are all handled by and incorporated into one financial or external ERP system that can give you running totals of costs, revenue, profit or loss, and even ROI calculations.
And on the HCP practice side, the system performs compliance management, Telehealth management, e-Prescriptions, and practice reporting. Features that may or may not be included are personnel management, hospital bed management, and pharmacy inventory management software. We take a look at these essential elements as a response to the query, what are medical practice management software requirements?

Key Medical Practice Management Software Requirements
Examples of Medical Practice Management Software
What are examples of Medical Practice Management Systems (MPMS)? Most MPMS are standalone products that have the standard features mentioned above and more. Some are generalist software, while others center more on certain medical practices, but all of them are customizable to your own practice. There are a few that are part of enterprise suites, integrated with CRM or ERP suites that are geared more for use by larger institutions. The leading MPMS products are as follows:
AthenaHealth
athenahealth is a US-based provider of network-enabled and cloud-based healthcare services, including point-of-care mobile apps for clinical practices, hospitals, or other medical organizations. It monitors patient outcomes, operational costs, billing, and all aspects of your medical practice. Among the organizations it has served are OBGYN, orthopedics, FQHCs, health plans, member-centric organizations, startups, and ancillary service organizations, with customers across 110 medical specialties.
Practice Fusion
Practice Fusion is a US-based EHR company specializing in small and independent practices. Its cloud-based system ensures no software to download or hardware to install, manage, and maintain, no associated fees, and EHR security and backup. It has a network of e-pharmacies, over 500 testing laboratories, and imaging centers, making patient lab tests, diagnosis, and e-prescriptions faster and more efficient.
Cerner EMR
Cerner EMR is a component of the Oracle suite of solutions that integrate clinical, financial, and operational tools to help produce improved patient outcomes and high-quality patient care. Its enterprise capabilities include contract management, claims and accounts receivables management, clinical reviews, and powerful analytics.
TherapyNotes
TherapyNotes is a cloud-based EMR specifically designed for behavioral and mental health, catering to solo psychologists or large teams of behavioral and mental health specialists, including therapists, psychiatrists, social workers, counselors, and other mental health professionals. Its main features include real-time eligibility checking of your clients’ insurance coverage, electronic remittance advice (ERA), client payment tracking, and built-in regulatory health data submission.
Sevocity
Sevocity is a cloud-based EHR medical solution and billing platform offering custom EHR solutions for more than 40 specialties and counting. Its greatest strength is customizability, allowing you to choose what components work best for you in your own practice management, coupled with your insurance providers’ preferences, you can mix and match PM and billing systems from other companies. It provides a free bi-directional interface to the PM system of your choice and will build custom interfaces for free.
Having outlined the answer to the query, what are medical practice management software requirements, we turn to look at what lies ahead for this crucial medical industry.
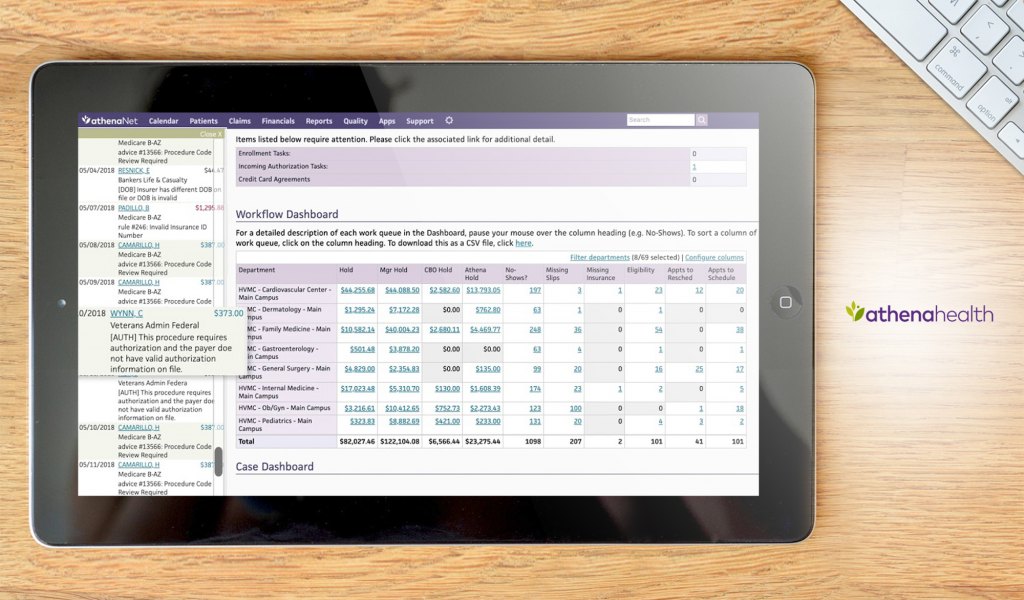
AthenaHealth provides reporting and analytics for metrics such as revenue, patient visits, and relative value units.
Medical Practice Management Software Requirements
So, what are medical practice management software requirements? The following list enumerates the very basic requirements for an MPMS, which may vary according to your location, practice type and size, business associates, facilities, number and type of personnel, regulations in your specific state or country, and other considerations.
1. Billing and Payment Processing
In most cases, patients do not pay hospitals or healthcare facilities directly but rely on insurance providers and government programs like Medicare or Medicaid. In Japan, the government pays for most costs, with patients paying only 30% of the total cost. The United States Affordable Care Act (ACA) enabled millions to gain insurance coverage.
Many countries offer universal health coverage, but often, the money is refunded after paying a large amount. In the US, under the Merit-Based Incentive Payment System (MIPS) for Medicare payment adjustments, clinicians may receive a payment bonus or payment penalty depending on CMS metrics.
Processing refunds, discounts, deductibles, copays, and coinsurance may become quite complicated, especially for large hospitals. It can become even more complex if the patient switches healthcare facilities and only paper documents are available.
Electronic Remittance Advice (ERA) transactions can also be complicated as they may cause adjustments to claims and payments to health care providers due to contract agreements, secondary health plans, patient benefit coverage, capitation payments, expected copays and coinsurance, risk adjustments, and IRS (Internal Revenue Service) tax withholding. A recent US physician survey revealed many problem areas related to these.
Source: 2022 MGMA Annual Regulatory Burden Report
Fortunately, several platforms have billing features that include fully-integrated clearinghouses for patient claims, unlimited claims and ERAs processing, statement processing, real-time A/R (accounts receivable) reporting, patient payment status monitoring, insurance provider payment status monitoring, and financial data generation. Patients and providers can be alerted by the system using e-mails and text, and real-time monitoring of payment status is automatically displayed on dashboards.
The top payer types accepted by most practices are private/commercial payers at 86%, followed by Medicare (70%) and Medicaid (73%). Veterans Affairs (41%) are utilized mostly by US veterans. This indicates the importance of integration and automatic handling of transactions and billing with these entities. Virtually all MPMS platforms are able to do this, differing only in degree of customizability.
Source: 2021 Telehealth Survey Report | American Medical Association
2. Regulatory Compliance
In the US, the Health Insurance Portability and Accountability Act of 1996 (HIPAA) is a federal law that imposes national standards for the protection of sensitive patient health information from being disclosed or used without a patient’s consent or knowledge.
Its three components are the Privacy Rule, the Security Rule, and the Breach Notification Rule. The Privacy Rule lays out the standards for the use and disclosure of protected health information (PHI), the Security Rule lists the required safeguards that should be taken by organizations, entities, and their business associates to secure electronic PHIs (ePHI), and the Breach Notification Rule requires the notification of affected individuals, HHS, and other relevant bodies of any breach or unsecured PHI data.
In a 2022 survey of HCPs regarding the degree of burden of some regulatory issues, they classified as very or extremely burdensome prior authorization, surprise billing and good faith estimate requirements, Medicare Quality Payment Program (MIPS/APMs), audits and appeals, and Medicare Advantage chart audits, among others.
Source: 2022 MGMA Annual Regulatory Burden Report
Other countries have their own similar versions of these rules: Canada has the Personal Information Protection and Electronic Documents Act (PIPEDA), the United Kingdom has the Data Protection Act, which has a wider scope, the European Union has its General Data Protection Regulation (GDPR), among other countries.
Thankfully, all MPM systems are HIPAA-compliant as a requirement for operating commercial licenses and for legal compliance. They mostly differ in terms of the degrees of customization of automation, reporting functions, and integrations with other systems, and your choice of a system may solely depend on these.
3. EHR Management
EHRs (electronic health records) are simply the digital version of a patient’s chart that includes patient demographics (name, date of birth, sex, identification, language, and ethnicity), patient contact information, and patient care-related information like primary provider, insurance coverage, HIPAA information, medical history, diagnoses, predispositions, drug therapy and prescription history, surgical history, family history, vaccination status and history, allergies, laboratory test results, medical or care facility movement history, address tracking, and other relevant information.
One advantage of EHRs is their ability to consolidate information from all clinics, medical, or home care facilities the patient has been to, and from all clinicians involved, presenting a more complete and accurate medical history profile, which aids in better diagnoses and treatments. All these can be done through secure online connections by authorized access only, allowing instant access to patient EHRs anywhere with an Internet or mobile connection. All EHRs are required to handle updated ICD-10 codes, and automatic EHR field input using partial text or code entry, which is extremely helpful to clinicians to prevent encoding errors.
Lack of EHR interoperability is a big problem among different EHR systems, so perhaps it would be better to go for an open data format or for systems that can import, interpret, and transform formats seamlessly. For more information, check out this list of the top 20 EHR software companies.
4. Analytics and Reports
Most systems are capable of displaying real-time analytics and reports on dashboards or as PDF documents, and many of them utilize artificial intelligence (AI) and real-time machine learning to learn more about your business workflows and identify areas for improvement.
Analytics’ predictive algorithms can be set to trigger alerts to providers to help make decisions on patient care in real time, especially for high-risk patients or those requiring intensive care. These were particularly useful during COVID-19 pandemic case surges where dashboards allowed stakeholders to visualize capacity and forecast future trends.
AI-enabled workflows enable data-driven models, further streamlining your practice. In addition, several platforms can provide you with a current financial snapshot of your complete revenue cycle, from accounts receivable to claims, billing, current profit and loss, and bottom line, all in real time.
Visualization via dashboards is a huge plus, allowing you to see how everything is in your medical practice and business at all times. You can also drill down into all components of operations to see where processes can be optimized and financial performance improved. From these, increased practice revenue will lead to higher quality standards and better patient outcomes.
5. Communication
Communication handling among patients, doctors, nurses, and other HCPs is essential to your practice.
Automated messaging, reminders, and notifications are pretty standard features in medical practice software encompassing text messages, e-mails, WhatsApp notifications, social media notifications, phone calls, and automated voice reminders.
In large hospitals with hundreds of patients, doctors, nurses, and many surgeries and procedures going on, it could be quite difficult to keep track of everything.
Fortunately, all MPMS platforms can do these with relative ease.

6. Claims Processing
In the US, the Merit-Based Incentive Payment System (MIPS) for Medicare payment adjustments allows eligible clinicians to receive a payment bonus or incur a payment penalty depending on several metrics. A system that can calculate these and automatically incorporate them into your billing statements and insurance reimbursements is essential as it is very tedious to track every single adjustment. It should also be easily programmable to incorporate country-specific metrics and policies into cost and billing calculations. Physicians sounded out their opinions on various aspects of MIPS.
Timely filing is also very important as insurance companies may deny very late claims. Real-time automated filings can greatly increase efficiency and your chances of getting reimbursed. Handling procedure codes with data entry validation for error-checking are also ideal to prevent mismatched entries and other clerical errors.
An ideal system should also expertly handle claims routing based on member, provider, location, and other factors, pre-adjudication clinical editing, auto-filling the correct claims forms, insurance plan matching, supplemental plan types, and expert data capture for claims, EOBs, bills, and other financial data. CMS and ERP platform integration is also desirable, especially for very large practices across several locations.
7. Patient Preregistration and Scheduling
In most cases, patients are allowed and even encouraged to schedule doctor appointments and are given the option to cancel or reschedule appointments. Tracking hundreds of these manually and through front-office personnel is very tedious and error-prone, so a system that handles automatic scheduling is essential to practices large or small. Electronic records also help easily review past patient appointments for audit and tracking purposes.
Patient preregistration has a lot of benefits, including pre-screening and prioritization of at-risk patients, matching patients with the right specialty doctors, determining insurance eligibility and status, contacting insurance providers for available discounts, other payments, and payment timelines, among others.
8. Telehealth
Telehealth has exploded during the COVID-19 pandemic and will likely increase or remain at current levels, according to physicians. In the US in 2021, 85% of physicians are currently utilizing telehealth with patients, either video or voice-only.
2021 AMA Telehealth Survey of Physicians
(percentage of respondents)
Physician respondents currently using telehealth: 85
Physician respondents currently using telehealth
%Telehealth - live, interactive video visits with patients : 93
Telehealth - live, interactive video visits with patients
%Telehealth - audio-only visits: 69
Telehealth - audio-only visits
%Telehealth has allowed our practice to provide more comprehensive quality care for patients: 60
Telehealth has allowed our practice to provide more comprehensive quality care for patients
%Patients have better access to care since they began using telehealth: 80
Patients have better access to care since they began using telehealth
%Physicians agree or strongly agree their patients are more satisfied since using telehealth: 62
Physicians agree or strongly agree their patients are more satisfied since using telehealth
%Telehealth has improved the satisfaction of their work: 54
Telehealth has improved the satisfaction of their work
%Telehealth decreased the costs of care (strongly agree or agree) : 44
Telehealth decreased the costs of care (strongly agree or agree)
%Patients are primarily located at their home at the time of the virtual visit: 95
Patients are primarily located at their home at the time of the virtual visit
%Source: 2021 Telehealth Survey Report | American Medical Association
Designed byServices currently provided via telehealth among small to large practices are medical management (e.g. medication management), chronic disease management, specialty care, mental/behavioral health, acute care/ urgent care/ same day care, preventative care or primary care, hospital or ED follow-up care, and acute care inpatient services. It only shows the importance of telehealth services to both patients and practice. All statistics show an increase in telehealth adoption, physician satisfaction with their jobs, patient access to healthcare, and a decrease in costs of care.
Before the pandemic, physicians were not fully convinced that telehealth was applicable to most types of patient care, but currently, almost all aspects of patient care are being conducted in the US via telehealth, namely, treatment or therapy, screening, assessments, diagnosis, follow-up care (e.g., post-surgical, chronic care, and post-hospitalization care), continuous patient monitoring, and even patient Intake and triage.
Source: 2021 Telehealth Survey Report | American Medical Association
Systems that are telehealth-enabled coupled with mobile phone apps will continue to evolve and be in demand, and it is expected that telehealth services will continue to markedly increase in the foreseeable future.
9. Patient Portal
The patient portal allows patients to check and update their medical records themselves, decreasing manual entry from your front-office staff and allowing for the double-checking of information, correcting misspellings and erroneous histories, updating data on movement from different care facilities, and updating insurance information.
They can also schedule appointments or choose their own doctors. It is well-known that the patient experience is very valuable and produces better outcomes.
Some systems link their portals to knowledge base article libraries where patients can read layman-friendly articles on diseases, their conditions, treatments, and therapies. These reduce self-medication errors and increase patient understanding of therapies or procedures. Online support communities that cater to the psychological side of patients are also gaining popularity.
10. Mobile Device Support
Practically most tasks and activities are done using mobile phones for both patients and HCPs. On the HCP side, wall-mounted kiosks or mobile devices allow staff to work freely and from any location, documenting the patient’s daily activities at or near the point of care. Smartwatches and IoT devices can be used as wireless data capture devices for patient vitals, oxygen saturation state, sleep/wake cycles, etc. These devices are increasingly being used because of their convenience and accuracy. Systems that can perform electronic data capture of these devices are quite advantageous, as discussed in the 20 best clinical trial management software.
For patients, everything from scheduling appointments, viewing and updating their medical records, and receiving billing statements to payments through mobile banking are done on their mobile phones. Most MPM systems have these capabilities, including telehealth services, though they may vary in the details.
11. Integrations
Many MPMS platforms are integrated with networks of e-pharmacies, clearinghouses, medical insurance providers, other healthcare facilities, and regulatory bodies and agencies, although they vary in coverage area and the number of institutions they have direct access to. Some platforms integrate with enterprise solutions like CRMs and ERP software for total organization-wide integration of all operations. Most of them can also integrate machine learning and AI with your data as it is captured in real time. APIs also allow you to incorporate your own scripts and apps in the MPMS directly.
12. Practice Reporting
Practice reporting is the automatic or manual reporting of new findings, new diseases, best practices, what your clinic is trying out (e.g., experimental last resort drugs), vaccination rates of patients, adverse drug events, psychological/mental health statistics of your patients, and other relevant clinical data to registries or regulatory agencies.
For example, the Mental and Behavioral Health Registry (MBHR) is a repository of quality outcomes in the practice of behavioral health, and submission of clinical data helps improve mental health interventions. Participating in immunization registry reporting is valuable to national health and disease tracking, as we all experienced during the COVID-19 pandemic. By submitting immunization data, you can receive immunization forecasts and histories from the government’s public health immunization registry.
Reporting medication errors should be easy and encouraged to improve healthcare; although this has had low participation rates because of fear of reprisals or gaining a bad reputation, systems should enable physicians to report adverse drug events, practice errors, and other information that will help improve the practice and regulatory policies.
13. e-Prescriptions
Most modern software systems allow you to send prescriptions to any e-prescribing-enabled pharmacy, and handling e-prescriptions for controlled substances (EPCS) have become more secure with two-factor authentication. Advanced features allow you to query drug stock inventory levels, consult formularies and drug adverse interaction databases, and formulate the cheapest and most efficient regimen, among others.
Statistics show that e-prescriptions rose steadily for controlled and non-controlled substances from 2017 to 2020, indicating its steady rise in popularity among prescribing doctors and pharmacists.
Source: Surescripts, 2021
You can also electronically request patient refills or generics substitutions when applicable. These features will increase your workflow efficiency and prescription accuracy, eliminating doctors’ handwritten prescriptions, which are often not legible. You can take advantage of a network of more than 100,000 e-prescription-enabled pharmacies in the US, giving you many choices.
14. Security
All MPMS platforms are HIPAA-compliant as a requirement for commercial license approval. HIPAA and other privacy laws are integrated into system design and implementation. You can set user roles with corresponding privileges to ensure only authorized access to EHRs and company data. Recent data on HIPAA-related entities show an increase in data breaches from 2017-2022, mostly from the healthcare providers’ end.
Source: HIPAA Journal, 2022
Cybersecurity incidents could threaten network-connected medical devices and data systems and may affect appointments and surgeries and cause the closure of care units or whole organizations, putting patients at risk. MPMS platforms that can perform automated, secure, and quick backup restoration of all data and systems are critical and should be your top IT priority.
Trends in Medical Practice Management Software
Clinical decision-support systems based on AI and machine learning, AI-generated diagnoses from scans, X-ray charts, MRI data, and other output are rivaling expert diagnoses, and in some cases, even outperforming them in difficult cases. AI models will only continue to improve with larger training datasets and expert-enabled supervised machine learning. We should view this technology as a helper that can make diagnosis quick and accurate, especially for rare, difficult, or early-stage diseases. This can save hospitals on treatment and in-patient boarding costs, especially if the diagnosis is made at the early stages of the disease.
Modern payment schemes have evolved from traditional reimbursement models toward value-based patient-centered health care, where quality and cost are of great importance. Patients have become more informed and aware and demand transparency and accountability. Payers and insurance providers are more particular about accountability for how the insurance money is being spent. With these changes, many practices have found it very difficult to keep up with changing regulations and incorporate these changes in their billing systems and EHRs without a powerful and customizable system. For more information, you can check the ten best billing software systems.
A persistent problem of HCP organizations is staffing shortages, and a survey of healthcare executives showed that COVID-19 has had lingering negative effects on staff satisfaction (72%) and staffing levels (84%). Poor staffing levels often lead to poorer patient outcomes and increases in hospital-associated infections, and hopefully, your MPMS can help alleviate these to some extent.
While ICD-10 codes are necessary and provide more details on diseases, treatment options, and medical devices, their sheer volume and specificity make it difficult to track everything manually, creating mismatches in data entry, which may delay payments, or worse, cause medical errors that may lead to worse outcomes. Systems that do these automatically are essential, not just desirable, to your practice.
























Leave a comment!